Definition of Acute Respiratory Distress Syndrome (ARDS):
ARDS (acute respiratory distress syndrome) may be defined as acute, diffuse pulmonary inflammatory response to either direct (via airway or chest trauma) or indirect blood-borne insults that originate from extra pulmonary pathology. It is frequently associated with other organ dysfunction (kidney, heart, gut, liver, coagulation) as a part of multiple organ failure.
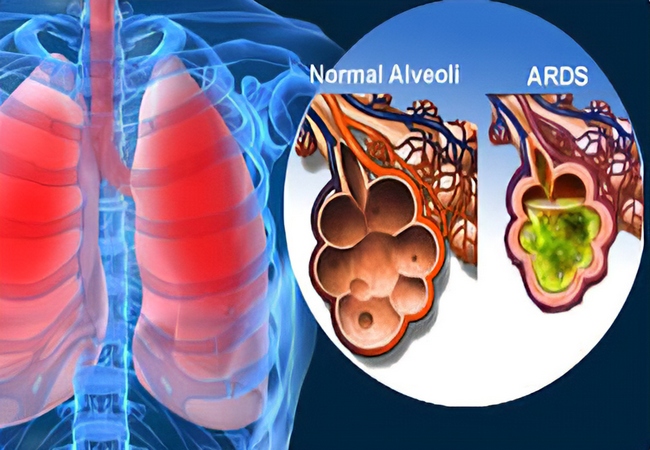
It is characterized by-
- Neutrophil sequestration in pulmonary capillaries.
- Increased capillary permeability, protein-rich pulmonary oedema with hyaline membrane formation.
- “Damage to type 2 pneumocytes leading to surfactant depletion.
- Alveolar collapse and reduction in lung compliance.
The criteria defining ARDS are:
- Hypoxaemia defined as Pa02/ F102( <200 mmHg).
- Chest radiograph showing diffuse bilateral infiltrates.
- Absence of a raised left atrial pressure.
- Impaired lung compliance.
Causes of ARDS /Conditions Predisposing to ARDS:
A. Inhalation (direct):
- Aspiration of gastric contents,
- Toxic gases/burn injury,
- Pneumonia,
- Blunt chest trauma,
- Near-drowning.
B. Blood-borne indirect):
- Sepsis,
- Necrotic tissue (particularly bowel),
- Multiple traumas,
- Pancreatitis,
- Cardiopulmonary bypass,
- Severe burns,
- Drugs (heroin, barbiturates, thiazides),
- Major blood transfusion reaction,
- Anaphylaxis (wasp, bee, snake venom),
- Fat embolism,
- Carcinomatosis,
- Obstetric crises (amniotic fluid embolus, eclampsia).
How will You Manage a Case of Acute Respiratory Distress Syndrome (ARDS)?
Management of Acute Respiratory Distress Syndrome (ARDS):
Clinical Features of Acute Respiratory Distress Syndrome (ARDS):
- Rapidly progressive dyspnoea,
- Tachypnoea.
- Central cyanosis, refractory to 02 therapy.
- Bilateral crepitation, inspiratory rhonchi
- Intercostal indrawing.
Investigation:
- Chest x-ray:
- Bilateral, diffuse fluffy shadow,
- Ground glass appearance in lung fields.
- Arterial blood gas analysis.
- Left atrial pressure measurement.
Treatment of Acute Respiratory Distress Syndrome (ARDS):
A. Supportive Rx:
a) Rest with propped up position
b) Oxygen inhalation with high inflation pressure & high conc. 02,
c) Positive end expiratory pressure (PEEP) by mechanical ventilation.
d) High dose of corticosteroid
e) Inhalation of nitric oxide may improve gas exchange.
B. Early & effective treatment of precipitating cause.
D/D:
- Acute left ventricular failure (LVF),
- Lung fibrosis.
Nursing Management of Acute Respiratory Distress Syndrome (ARDS):
Nursing assessment:
- Assess and note dyspnea, tachypnea, internal-muscular traction, fatigue, or pulmonary edema.
- Assess breath sounds.
- Assess the level of consciousness and ability to tolerate increased work of breathing,
- Assess the signs of hypoxemia and hypercapnia.
Nursing diagnosis:
- Ineffective breathing pattern,
- Impaired Gas Exchange,
- Ineffective airway clearance,
- Decreased Cardiac Output,
- Risk for Injury,
- Excess Fluid Volume,
- Impaired Verbal Communication,
- Impaired Physical Mobility,
- Impaired Skin Integrity,
- Sleep Pattern Disturbance,
- Ineffective Coping.
Expected outcomes:
- Stating/show loss of dyspnea.
- Maintain a patent airway with breath sounds clean / no crackles.
- Issued a secret without difficulty.
- Show behavior to improve/ maintain airway clearance.
Nursing intervention:
- Maintain a patent airway by suctioning. Use sterile, non-traumatic technique.
- Ensure adequate humidification to help liquefy tenacious secretions.
- Provide any other means of communication for the patient on mechanical ventilation.
- Gives sedatives as ordered to reduce restlessness.
- Reposition the patient often. A high fowler position may be needed.
- Note and record any changes in respiratory status, temperature, or hypotension that may indicate a deteriorating condition.
- Record caloric intake. Administer tube feedings and parenteral nutrition as ordered.
- To promote health and prevent fatigue, arrange the alternate periods of rest and activity.
- Maintain joint mobility by performing passive range-of-motion exercises.
- Provide meticulous skin care to prevent skin breakdown.
- Provide emotional support.
- Monitor the patient’s level of consciousness, noting confusion or mental sluggishness.
- Closely monitor the patient’s heart rate and blood pressure
- Frequently evaluate the patient s serum electrolyte levels.
- Monitor and record the patient’s response to medication.
- Evaluate the patient’s nutritional intake.

Maria Khatun Mona is a Founder and Editor of Nursing Exercise Blog. She is a Nursing and Midwifery Expert. Currently she is working as a Registered Nurse at Evercare Hospital, Dhaka, Bangladesh. She has great passion in writing different articles on Nursing and Midwifery. Mail her at “maria.mona023@gmail.com”
