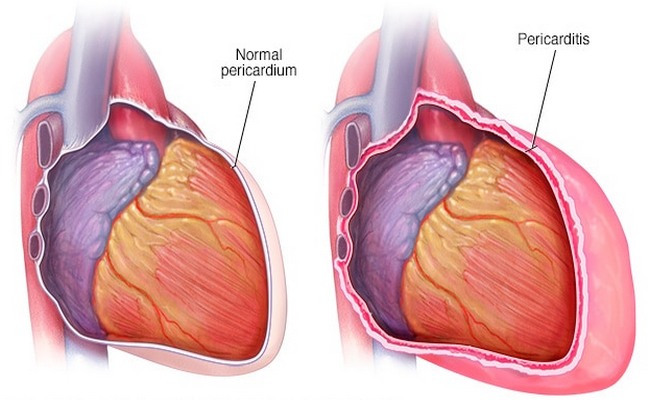
Pericarditis Definition:
The pericardium is a thin, two-layered fluid-filled sac that covers the outer surface of the heart. Pericarditis disease is an inflammation of the pericardium. Pericarditis usually begins suddenly but does not last long.
Causes of Pericarditis Disease:
There are different types of reasons for pericarditis disease which are the following:
1. Infection:
- Viral (Coxsackievirus B, A, Adenovirus, Mumps),
- Bacterial (Pneumococci, Staphylococci, Streptococci, Septicemia),
- Fungal (Histoplasma, Candida Species, Infections such as toxoplasmosis,
- Lung disease (Tuberculosis),
- HIV (Human Immunodeficiency Virus).
2. Non-Infection:
- Uremia,
- Radiation-Induced,
- Myxedema,
- Acute MI,
- Dissection of Aortic Aneurysm,
- Trauma to the heart (Thoracic Surgery pacemaker),
- Delayed post-myocardial- pericardial Injury,
- Post cardiac syndrome,
- Post myocardial infarction syndrome,
- Side affects some medication such as Isoniazid, cyclosporine, Tetracycline,
- Malignancy,
- Scleroderma,
- Ankylosing spondylitis,
- Inflammatory bowel disease,
- Rheumatic fever,
- Immunologic (Systemic lupus very tomatoes, Rheumatic fever),
- Cancer (including leukemia).
Sign and Symptoms of Pericarditis Disease:
Various signs and symptoms of pericarditis disease are mentioned below:
- Sharp, Stabbing Chest pain over the center or left side of the chest,
- Trouble breathing when lean back or in a relaxed position,
- Pulse and BP difference in upper extremities,
- Palpitations,
- Weakness,
- Coughing,
- Hoarseness, voice weakness or complete aphonia,
- Dysphagia,
- Cyanosis,
- Distended neck veins,
- Anxiety and fatigue,
- Low-grade fever,
- Abdominal or leg swelling for long term pericarditis.
Test and Diagnosis for Pericarditis Disease:
There are different test and diagnosis systems for pericarditis disease, which are in the following:
- Medical history and physical exam,
- ECG,
- Echocardiography,
- Cardiac CT scan/ MRI,
- Blood test- C-reactive protein (CRP), Blood Urea Nitrogen (BUN), Troponin-I, CK-MB, Myoglobin, ESR.
- Radionuclide scanning.
Treatment for Pericarditis Disease:
Various treatments for pericarditis are below:
- Antibiotic (To treat bacterial infection),
- Antifungal medicines will be used for fungal pericarditis,
- Non-Steroidal anti Inflammatory Drug (to reduce pain and inflammation),
- Diuretics ( to remove excess fluid),
- Pericardiocentesis (To drain the excess fluid from pericardium),
- Pericardiectomy (In case of constrictive pericarditis),
- Hemodialysis (To treat uremic pericarditis),
- Antipyretics,
- Analgesics.
A complication of Pericarditis Disease:
Different complications of pericarditis are in the following:
- Pericardial effusion,
- Constrictive pericarditis,
- Cardiac tamponade,
- Fatal hemorrhage,
- Myocardial ischemia,
- Stroke,
- Paraplegia due to interruption of the anterior spinal artery,
- Abdominal ischemia.
Nursing Intervention for Pericarditis Disease:
There are various types of nursing intervention for pericarditis, those are mentioned below:
- Monitor patient pain level and evaluate pain within 30 minutes.
- Administer prescribed pain medication such as morphine to relieve pain.
- Monitor the patient pain level and effectiveness of analgesics.
- Provide a comfortable position (sit up and lean forward).
- Check vital signs and record them continuously.
- Discuss disease process and signs and symptoms expanding aneurysm or impending aneurysm.
- If surgical intervention is needed, provide psychological support, and prepare for surgery.
- For post-surgical patients, discuss warning signs of postoperative complications such as fever, inflammation in the surgical site, bleeding, and swelling.
- Daily check of weight.
- Closely monitor and notify a physician about persistent cough, vomiting, or systolic blood pressure above 180mmhg because of the increased risk for hemorrhage.
- Ensure bed rest until fever, chest pain and friction rub disappear.
- Administer O2 and keep SPO2 ˃90%.
- Administer medication as order-such as NSAIDs and steroids with food.
- Ensure administer of antibiotic timely.
- Continue I.V antihypertensive medication if persistent blood pressure high.
- Carefully maintain fluid intake and output.
- Reassure the patient that chest pain is not a Myocardial Infarction.
- Check signs and symptoms for cardiac tamponade at least 8 hourly and PRN.
- Assist the patient with bathing if necessary.
- Provide a bedside commode to reduce stress on the heart.
- Tell the patient to resume his daily activities slowly.
- Build a rapport relationship with the patient to reduce anxiety.
More questions related to this topic:
- Pericarditis: Get Facts on Causes Symptoms and Treatment.
- Pericardial Disease: Diagnosis and Management.
- What is Pericarditis?
- What is the Meaning of Pericarditis?
- What is Inflammation Around the Heart?
- What is the Disease of Pericardium?
- Definition of Pericarditis Disease.
- Pericarditis Heart disease.
- Pericarditis Cancer.
- Pericarditis Symptoms.

Maria Khatun Mona is a Founder and Editor of Nursing Exercise Blog. She is a Nursing and Midwifery Expert. Currently she is working as a Registered Nurse at Evercare Hospital, Dhaka, Bangladesh. She has great passion in writing different articles on Nursing and Midwifery. Mail her at “maria.mona023@gmail.com”

Greetings, Maria. My name is Rachel Banda and I have been assigned to do a small power point presentation on Pericarditis. I am asking permission if I could use the image and part of your article on this?
Yes, But you have to mention our website address in that presentation. Thanks.