Definition of Ventricular Fibrillation (VE):
Ventricular fibrillation is ventricular arrhythmia characterized by very rapid and irregular, 1netfective &uncoordinated ventricular activation with no mechanical effect. It is the commonest causes of sudden death.
Causes of Ventricular Fibrillation (VE):
It includes-
- Acute MI,
- Electrolyte imbalance especially hypokalemia,
- Electrocution,
- Drug overuse (Digitalis & adrenaline),
Clinical Features of Ventricular Fibrillation (VE):
- History of ischemic heart disease.
- History of taking anti-arrhythmic drug.
- The patient becomes rapidly unconscious and is pulseless.
On examination:
- Pulse-Absent,
- BP-Non recordable,
- Respiration-Ceases/absent,
- Pupil-Dilated, less or no reaction to light,
- Heart sound-Absent.
Investigations:
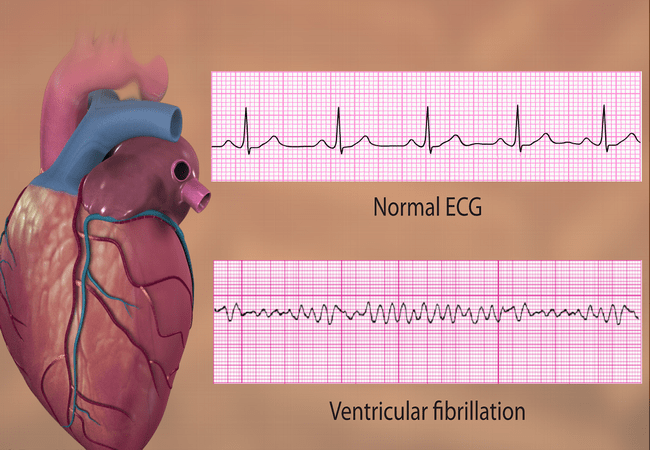
ECG- It shows chaotic, bizarre, irregular ventricular complex.
Treatment of Ventricular Fibrillation (VE):
- Defibrillation is the only effective treatment for ventricular fibrillation.
- Defibrillation with biphagic shock of 150 joules.
- If normal rhythm is not restored, a further shock of 150-200 joules is given.
- If unsuccessful, a 3rd shock of 150-200 joules is given.
- If these 3 shocks are unsuccessful then.
- 1 mg of adrenaline IV & a further 1 min of cardio-pulmonary resuscitation are given before trying a further sequence of up to 3 shocks each at 150-200 joules.
Nursing Management of Ventricular Fibrillation:
- Avoid causing intense emotional situations.
- Avoid too hot cold patient.
- Prevents decision making when patients are under severe stress.
- Refrain from giving oral stimulants.
- Refrain from entering anal lubricant.
- Refrain from taking rectal temperature.
- Refrain from doing a rectal or vaginal examination.
- Limit environmental stimuli.
- Delays shower if appropriate.
- Restrict smoking.
- Encourage competitive.
- Instruct the patient to progressive exercise.
- Instruct the patient or family on the symptoms of heart compromise shows need for rest.
- Patient identity method of handling stress.
- Perform relaxation therapy if appropriate.
- Monitor patients for self-care ability,
- Monitor patient’s need for adaptive devices for personal hygiene, dressing, toileting, and eating.
- Provide the desired personal article.
- Provide assistance until the patient is fully able to assume self-care.
- Assist patients in receiving the dependency needs.
- Use a consistent repetition of routine health care as a way of setting them.
- Encourage independence, but the intervention when the patient cannot perform.
- Teach parents or family to encourage self-reliance, to increase only when the patient i1 unable to perform.
- Establish a routine for self-care activities.
- Consider patient age when promoting self-care activities.

Maria Khatun Mona is a Founder and Editor of Nursing Exercise Blog. She is a Nursing and Midwifery Expert. Currently she is working as a Registered Nurse at Evercare Hospital, Dhaka, Bangladesh. She has great passion in writing different articles on Nursing and Midwifery. Mail her at “maria.mona023@gmail.com”
