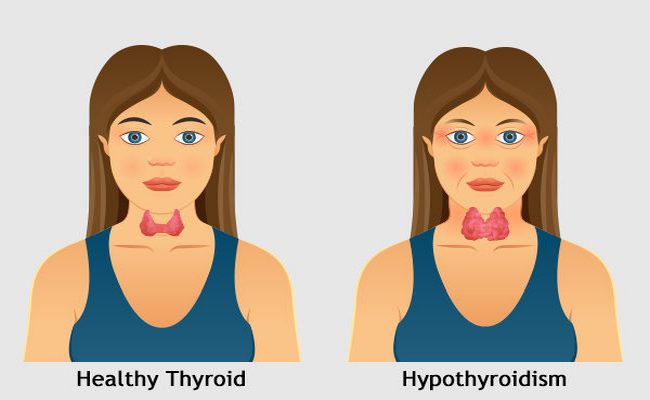
Definition of Hypothyroidism:
A Clinical condition characterized by subnormal level of circulating thyroid hormones. It associated with generalized non pitting ordema is called myxocdema.
Classification of Hypothyroidism:
1. Primary: Here the abnormality is within thyroid gland, either structural or functional.
2. Secondary: Here the abnormality is in the hypothalamic-pituitary axis resulting in decreased production of TSH.
In another classification:
Goitrous: Associated with enlargement of thyroid gland.
Nongoitrous: Not associated with enlargement of thyroid gland.
Causes of Hypothyroidism:
1. Autoimmune:
- Hashimoto’s thyroiditis,
- Spontaneous atrophic hypothyroidism,
- Graves’ disease with TSH receptor-blocking antibodies.
2. latrogenic :
- Radioactive iodine ablation,
- Thyroidectomy,
- Drugs : Lithium, Carbimazole, methimazole, propylthiouracil , Amiodarone.
3. Transient thyroiditis:
- Subacute (de Quervain’s) thyroiditis,
- Post-partum thyroiditis.
4. Iodine deficiency: e.g. In mountainous regions
5. Congenital:
- Dyshormonogenesis,
- Thyroid aplasia.
6. Infiltrative:
- Amyloidosis,
- Riedel’s thyroiditis,
- Sarcoidosis etc.
7. Secondary hypothyroidism: TSH deficiency
Management of Hypothyroidism:
Clinical feature of Hypothyroidism:
- Fatigue,
- Increased sensitivity to cold,
- Constipation,
- Dry skin,
- Weight gain,
- Puffy face,
- Hoarseness,
- Muscle weakness,
- Elevated blood cholesterol level,
- Muscle aches, tenderness and stiffness,
- Pain, stiffness or swelling in your joints,
- Heavier than normal or irregular menstrual periods,
- Thinning hair,
- Slowed heart rate,
- Depression,
- Impaired memory.
Investigation of Hypothyroidism:
1. Thyroid function tests:
- Total T4 & T3: T4 & T3 – decreased,
- TSH- increased,
- Free T4 & T3 – decreased.
2. Antithyroid antibodies:
- Antimicrosomal /peroxidaseAb,
- Antithyroglobulin ab.
3. Thyroid scan, USG, FNAC.
4. Routine exam: Rx:
- CBC- Anaemia,
- Serum cholesterol & TG : Raised,
- Urine R/M/E,
- X- ray chest : Cardiomegaly,
- ECG (>40 yrs): Low boltage ECG,
- Ischacmia,
- Bradycardia,
- X-ray neck lateral and A/P view V Retrosternal extension,
- Serum Na+ level: – decreased,
- Serum enzymes: Raised AST, CK & LDH.
Rx:
1. Oral thyroxin single dose/day.
Replacement dose:
- 50 ug0.05 mg daily & then increased,
- 1st 3 wks -50 µg once daily,
- 2nd 3 wks – 100 µg once daily,
- Lifelong — 150 µg once daily.
Hypothyroidism with IHD: Start with low dose such as 25 µg day.
2. If rapid response is required, tri-iodothyronine 20 µg 3 times daily.
Follow up:
Regular thyroid function test -6 weekly & adjust thyroxin dose.
Once the dose of thyroxin is established – thyroid function test-1-2 yearly.
Difference Between Hypothyroidism and Hyperthyroidism:
Points of Difference | Hypothyroidism | Hyperthyroidism |
About | Also known as over active thyroid. | Also known as underactive thyroid. |
Most Common Cause | Graves’ disease, also | Hashimoto’s disease, |
Other Causes | Thyroiditis, iodine | Thyroiditis, too much |
Diagnosis | Thyroid-stimulating | Thyroid-stimulating |
Treatment | Antithyroid medication | Synthetic thyroid |
Occurrence | Less common. Roughly | More common. Nearly |
Appetite | Weight loss but | Weight gain but loss |
Pulse | Tachycardia | Bradycardia |
Skin | Warm and moist | Dry and coarse |
Hair | Fine and soft | Thin and brittle |
Temperature | Heat intolerance | Cold intolerance |

Maria Khatun Mona is a Founder and Editor of Nursing Exercise Blog. She is a Nursing and Midwifery Expert. Currently she is working as a Registered Nurse at Evercare Hospital, Dhaka, Bangladesh. She has great passion in writing different articles on Nursing and Midwifery. Mail her at “maria.mona023@gmail.com”
