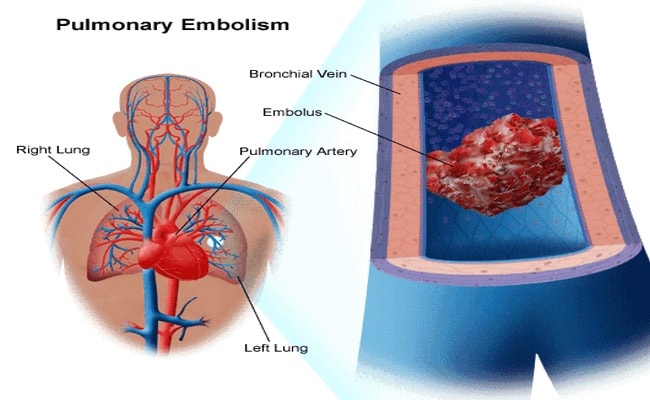
Definition of Pulmonary Embolism Disease:
Pulmonary embolism disease is a sudden blockage of the pulmonary arteries or one of its branches usually by a blood clot that travels to the lung from a vein in the leg.
Causes of Pulmonary Embolism Disease:
There are different types of causes for pulmonary embolism disease, those are mentioned below:
- A blood clot that forms in a deep vein in the leg,
- Small masses of infections material,
- Air bubbles,
- Fat droplet originate from narrow of a broken long bone,
- Part of a tumor,
- Amniotic fluid.
Risk Factors for Pulmonary Embolism Disease:
Various types of risk factors for pulmonary embolism disease are the following:
- Hospitalization or prolonged bed rest,
- Long time travel (Sitting in an Airplane, Train, etc.),
- Smoking,
- Major surgery (particularly involving the abdomen, pelvis, hip, or legs),
- Heart disease,
- Heart attack/failure,
- Lung disease,
- Previous history of DVT or PE,
- Inherited clotting disorders,
- Age (risk increases as age increases),
- A catheter located in a central vein,
- inflammatory bowel disease (Crohn’s disease or ulcerative colitis),
- Use of birth control pill,
- Overweight,
- Cancer,
- Pregnancy (Postpartum period up to 6-8 weeks after delivery),
- Leg paralysis,
- Varicose vein,
- Trauma to the vessel wall.
Sign and Symptoms for Pulmonary Embolism Disease:
There are different types of sign and symptoms for pulmonary embolism, those are mentioned below:
- Sudden shortness of breath,
- Sudden sharp chest pain,
- Cough with blood or mucus,
- Excessive sweating,
- Rapid or irregular heart rate,
- Palpitations,
- Dizziness or lightheadedness,
- Fainting,
- Cyanosis (Clammy or discolored skin) or mucous membranes,
- Sign of circulatory collapse (shock),
- Restlessness and anxiety,
- Dyspnea.
Test and Diagnosis for Pulmonary Embolism Disease:
Different ways of test and diagnosis systems for pulmonary embolism heart disease are given in the following:
- Chest X-Ray,
- Blood test (D-Dimer, ABG, Brain natriuretic peptide (BNP), Troponin-1),
- Ultrasound of chest,
- CT Scan of the chest,
- CT pulmonary angiogram,
- MRI,
- Echocardiogram (Echo),
- Electrocardiogram (ECG),
- Duplex ultrasound to see the structure of your leg veins,
- Venography.
Treatment for Pulmonary Embolism Disease:
There are different ways of treatment for pulmonary embolism, which are mentioned below:
1. Anticoagulants (Heparin, Warfarin):
Prevent forming new clots and prevent existing blood clots to grow larger.
2. Thrombolytic (Streptokinase or tissue-type plasminogen activators (t-PA) Reteplase, Urokinase interfere with the action of thrombin):
To dissolve or break up a blood clot quickly.
3. Embolectomy:
A Surgery help to remove the blood clot from the lung.
4. Vana cava filter:
Set a filter into the inferior vena cava. It helps to prevent blood clots reach the lungs.
Prevention for Pulmonary Embolism Disease:
Various ways to prevent ions for pulmonary embolism are given below:
- Daily use of anticoagulant medications.
- Wear compression stocking or use compression devices while hospitalization.
- Early ambulation or mobilization after surgery.
- Perform simple leg exercises and a short walk.
- During travel the following instructions should be maintained:
- Take a break from sitting and walk every couple of hours during travel.
- Flex ankles every 15 to 30 minutes.
- Do not sit with legs crossed at the knees for a long time.
- Wear flight socks.
- Drink plenty of water.
- Do not drink alcohol or take sleeping pills.
Nursing Intervention for Pulmonary Embolism Disease:
There are different types of nursing interventions for pulmonary embolism; those are mentioned in the following:
- Maintain client on bed rest strictly in a semi-flowers position and passive range of motion.
- Immobilize the patient and keep sit the head of the bed, but do not sit up.
- Keep elevated of the leg to promote a venous return to the heart.
- Check ABGs to evaluate the need for mechanical ventilation.
- Provide oxygen therapy and maintain ventilation as ordered.
- Establish an Intravenous line for fluids and drugs.
- Monitor vital signs continuously and record them carefully.
- Monitor and record intake and output to detect fluid overload and renal perfusion.
- Ensure a minimum intravenous fluid intake of 2500ml per day for proper hydration unless contraindicated to prevent increase blood viscosity.
- Administer heparin to reduce the risk of additional clotting.
- Carefully calculating heparin dose and use an infusion pump.
- Monitor laboratory test results such as partial thermoplastic time (PTT) to need of adjustment dose or stop heparin.
- Carefully monitoring of any complications such as hypotension, bleeding, desaturation, etc.
- Check any sign of hypotension and start inotropes as ordered and check ABP (Arterial blood pressure).
- Administer morphine to slow respiration and manage pain.
- Ensure intake of vitamin-k rich food including green, leafy vegetables to prevent bleeding.
- Advise the patient to take care when brushing teeth in order to reduce the risk of bleeding gums.
- Instruct patient to keep nasal mucosa hydrated and moist.
- Provide adequate knowledge to the patient pertaining to warfarin therapy.
- Check any sign of an excessive bleeding complication of warfarin therapy.
- Be aware of the signs of excessive bleeding, such as frequent and bilateral epitasis, hematuria (blood in the urine), and deep tissue bruising (Purpura).
More questions related to this topic:
- Pulmonary Embolism: Symptoms and Treatment.
- Pulmonary Embolism: Take Measures to Lower Your Risk.
- Pulmonary Embolism: Symptoms, Signs, Causes & Treatment.
- Pulmonary Embolism: Causes, Symptoms & Diagnosis.
- Pulmonary Embolism-Topic Overview.
- What is a Clot in the Lung?
- How do They Treat a Blood Clot in the Lung?
- What is an Acute Pulmonary Embolism?
- Pulmonary Embolism Heart Disease.
- Pulmonary Embolism Cancer.
- Pulmonary Embolism Diabetes.
- Pulmonary Hypertension Disease.
- Pulmonary Embolism Definition.
- Pulmonary Embolism Causes.
- Pulmonary Embolism Symptoms.
- Pulmonary Embolism Treatment.

Maria Khatun Mona is a Founder and Editor of Nursing Exercise Blog. She is a Nursing and Midwifery Expert. Currently she is working as a Registered Nurse at Evercare Hospital, Dhaka, Bangladesh. She has great passion in writing different articles on Nursing and Midwifery. Mail her at “maria.mona023@gmail.com”

I’ve recently been diagnosed with multiple pulmonary embolism and and is place on bedrest and clexane injections which I administer myself. My thing is, if this medication is only to prevent new clots and stop these from growing how do we get rid of the ones I have now. How do those disappear or disintegrate and make me healthy again???