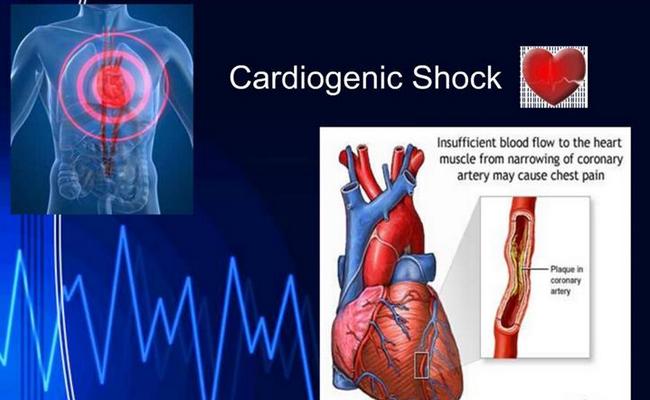
What Do You Mean by Cardiogenic Shock?
Cardiogenic shock is a condition in which the heart suddenly can’t pump enough blood to meet the body’s needs. The condition is most often caused by a severe heart attack. Cardiogenic shock is rare, but it’s often fatal if not treated immediately.
Sign and Symptoms of Cardiogenic Shock:
Cardiogenic shock signs and symptoms include:
1. Symptoms of Cardiogenic Shock:
As many patients with cardiogenic shock have had an acute MI, symptoms can include:
- Chest pain,
- Nausea and vomiting,
- Dyspnoea,
- Profuse sweating,
- Confusion/disorientation,
- Palpitations,
- Faintness/syncope.
2. Signs of Cardiogenic Shock:
It includes-
- Pale, mottled, cold skin with slow capillary refill and poor peripheral pulses.
- Hypotension (remember to check BP in both arms in case of aortic dissection).
- Tachycardia/bradycardia.
- Raised JVP/distension of neck veins.
- Peripheral oedema.
- Heaves, thrills or murmurs may be present and may indicate the cause.
Causes of Cardiogenic Shock:
Due to an intrinsic heart problem:
- MI,
- Myocardial contusion (often from steering wheel impact).
- Acute dysrhythmia compromising cardiac output.
- Acute mitral regurgitation (usually as a complication of MI due to ruptured chordae tendinae).
- Ventricular septal rupture (usually occurring as post-MI complication).
- Cardiac rupture (rupture of the wall of the left ventricle can occur post-MI or due to cardiac trauma).
- Hypertrophic obstructive cardiomyopathy or end-stage cardiomyopathy of other cause.
- Myocarditis.
- Post-cardiac surgery requiring prolonged cardioplegia and cardiopulmonary bypass.
- Severe valvular heart disease, particularly aortic stenosis.
Due to other causes:
- Acute, severe pulmonary embolism (PE)
- Pericardial tamponade or severe constrictive pericarditis.
- Tension pneumothorax.
- Myocardial suppression due to bacteraenmia or sepsis (although, strictly speaking, this may be defined as septic shock).
Nursing Management of a Patient with Cardiogenic Shock:
1. Initial management:
a) Administer oxygen by face mask or artificial airway to ensure adequate Oxygenation of tissues.
b) Adjust the oxygen flow rate to higher or lower level, as blood gas measurements indicate.
c) Asses vital signs strictly.
d) Assess functioning of ECG monitoring and readings.
2. Administering medications and IV fluids:
a) Administer an osmotic diuretic, such as mannitol, if ordered to increase renal blood flow and urine output.
Medications in choice-
- Dobutamine,
- Nitroglyserine,
- Dopamineohe.
Vasoactive medications-
- Epinephrine,
- Nor-epinephrine,
- Vasopressin.
b) Monitor vitals before and after administering medications and IV fluids.
c) Assess IV infusion site for bleeding or any allergic reaction.
d) Monitor Urine output, BUN and Serum creatinine.
3. Strict monitoring:
a) Monitor and record blood pressure, pulse, respiratory rate, and peripheral pulse eve- 1 to 5 minutes until the patient stabilizes.
b) Record hemodynamic pressure readings every 15 minutes.
c) Monitor ABG values, complete blood count, and electrolyte levels.
d) During therapy assess skin color and temperature and note any changes. Cold and clammy skin may be. a sign of continuing peripheral vascular constriction, indicating progressive shock.
4. Limit myocardial oxygen demand by-
a) Administer analgesics, sedatives, and other agents as prescribed.
b) Positioning the patient as comfort.
c) Limiting activities
d) Providing calm and quiet environment.
5. Emotional support and health maintenance:
a) To ease emotional stress, allow frequent rest periods as possible.
b) Offering support to reduce anxiety
c) Teaching the patient about his condition.
d) Allow family members to visit and comfort the patient as much as possible.

Maria Khatun Mona is a Founder and Editor of Nursing Exercise Blog. She is a Nursing and Midwifery Expert. Currently she is working as a Registered Nurse at Evercare Hospital, Dhaka, Bangladesh. She has great passion in writing different articles on Nursing and Midwifery. Mail her at “maria.mona023@gmail.com”
