Definition of Pulmonary Tuberculosis Disease (TB):
Pulmonary tuberculosis disease (TB) is a contagious bacterial infection that usually attacks the lungs. TB mainly affects the lungs. However, it affects any part of the body including the lymph node (Small glands), bones, digestive system, and nervous systems. It is called extrapulmonary tuberculosis disease (ETB).
Pulmonary tuberculosis disease is a treatable and curable disease if treatment continues in the right way.
Types of Pulmonary Tuberculosis Disease (TB):
There are two types of pulmonary tuberculosis disease (TB), which are discussed in the following:
1. Latent TB:
A tuberculosis bacterium presents in the body but cannot make/arise symptoms due to an active immune system. Immune systems are keeping it from turning into active TB and the disease goes to sleep is called Latent TB.
2. Active TB:
The bacterial grow fast and create symptoms against immune systems.
Causative Organism:
The bacteria of Tuberculosis are Mycobacterium Tuberculosis (TB).
Risk Factors of Pulmonary Tuberculosis Disease (TB):
There are different types of risk factors for pulmonary tuberculosis disease (TB), those are mentioned below:
- Children,
- Aged people,
- Malnourished people,
- Smoker and drug user,
- Immune compromised people such as HIV/AIDS, chemotherapy, diabetes,
- Overcrowded and unhygienic living area,
- International travelers,
- Health care provider.
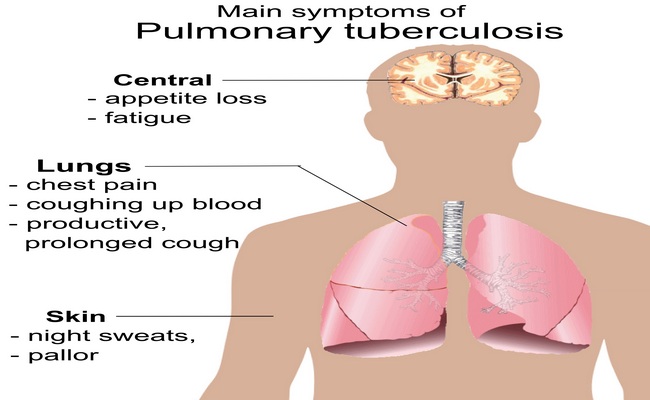
Sign and Symptoms of Pulmonary Tuberculosis Disease (TB):
Various types of sign and symptoms of pulmonary tuberculosis disease (TB) are given in the following:
- A persistent cough that lasts more than 3 weeks,
- Cough with cloudy and thick sputum,
- Coughing up blood,
- Consistent low-grade fever at night,
- Excessive sweating,
- Unexplained weight loss,
- Fatigue and tiredness,
- Rapid heartbeat,
- Swelling in the lymph nodes,
- Shortness of breath,
- Chest pain.
Mode of Transmission:
- TB bacteria can be transmitted through cough, sneeze, and the spit of an infected person.
- TB is an air-bone disease (Droplet).
- A single sneeze can release up to 40000 droplets and each droplet can transmit into the disease.
- TB bacteria can be live 6-7 hours in the air.
Test and diagnosis for Pulmonary Tuberculosis Disease (TB):
There are different types of test and diagnosis for pulmonary tuberculosis disease (TB), those are in the below:
- Chest X-Ray,
- Sputum culture for AFB (Acid-fast bacilli),
- Mantoux tuberculin test,
- IURAS (Interferon Gamma Release Assays),
- Chest CT Scan,
- Bronchoscopy,
- Biopsy,
- Lumbar puncture,
- Thoracentesis,
- Urine culture.
Treatment for Pulmonary Tuberculosis Disease (TB):
Various treatment ways for pulmonary tuberculosis disease (TB) are discussed in the following:
Treatment for Latent TB:
- In latent TB one antibiotic can use to kill the bacteria and prevent active TB.
- Isoniazid is a standard treatment for latent TB and needs to continue for 9 months.
- For people who cannot take Isoniazid for 9 months, sometimes a 6-month program is done.
- Rifampicin for 4 months is another acceptable treatment where Isoniazid is exposed to bacterial resistance.
Sometimes two antibiotics are used to treat latent TB. Treatment plan two antibiotics must be taken once a week for 12 weeks. The antibiotic combination includes Isoniazid and Rifapentine or Isoniazid and Rifampin.
Treatment for Active TB:
1. Anti- TB drug:
- Rifampicin,
- Isoniazid,
- Pyrazinamide,
- Ethambutal.
Combination of All 4 Anti-TB drugs to be used for six months as the standard recommended treatment or Active TB treatment
- First two months combination of Rifater (Isoniazid, Rifampin, and Pyrazinamide).
- Only Rifampin (Rifamate, Rimactane); and Isoniazid for the last four months. If Isoniazid resistance, Ethambutal or Streptomycin can be added.
2. Direct observation therapy.
Stopping treatment or skipping doses can make TB resistant to medicines, leading to developing Multi-Drug Resistant TB (MDRTB). It is a dangerous condition and difficult to treat.
Prevention for Pulmonary Tuberculosis Disease (TB):
There are different ways of prevention for pulmonary tuberculosis disease (TB), those are mentioned below:
- Avoid spending long periods of time in enclosed rooms with anyone who has active TB until that person has been treated for at least 2 weeks.
- Use protective measures and cover the face with an n-95 mask.
- Avoid direct face to face contact and maintain a safe distance.
- Carefully dispose of the infected persperson’stum in a covered bin.
- Maintain standard hand hygiene after any work of the TB patient.
- Avoid sharing personal belongings with an infected person.
- Use a negative pressure room where infected air out those rooms regularly.
- If someone lives with an active TB patient, help and encourage the person to follow treatment instructions.
- People who have been exposed to TB should have a skin test as soon as possible and have a follow-up test at a later date if the first test is negative.
- BCG vaccination to prevent TB. But, the effectiveness of this vaccine is limited.
A complication of Pulmonary Tuberculosis Disease (TB):
Various types of complications for pulmonary tuberculosis disease (TB) are given in the below:
- Aspergilloma,
- Arterial pseudoaneurysms,
- ARDS (Acute Respiratory Disease Syndrome),
- Bronchiectasis,
- Bronchopleural fistula Haemoptysis,
- Pneumothorax or Fibrothorax,
- Pleurisy,
- Pleural effusion,
- Empyema,
- Extensive lung destruction,
- Endobronchitis,
- Cor pulmonale,
- Ca bronchus,
- Immune Reconstitution Inflammatory Syndrome (IRIS),
- Laryngitis,
- Miliary Tuberculosis,
- HIV related opportunistic infections.
Nursing Intervention for Pulmonary Tuberculosis Disease (TB):
There are different types of nursing interventions for pulmonary tuberculosis disease (TB), those are described below:
- Place the patient in a negative pressure room
- Always keep the door of the patient’s room shut and place an isolation sign at a visible location.
- Monitor negative pressure is maintaining – 2mmhg.
- Use standard precautions and wear gloves, gowns when providing direct care to the patient.
- Maintain effective hand wash after giving care to patients.
- Nurse and visitors must wear an N-95 mask while entering the patient room.
- Dispose of all PPE (Personal Protective Equipment) carefully in the different colored bin.
- Provide isolation care until the patient is no longer contagious.
- Check vital signs regularly.
- Assess dyspnoea, tachypnea, and abnormal respiratory sounds.
- Always check sputum for blood or purulent expects ration.
- Encourage the patient to expectorate mucus and cough effectively.
- Keep patient in high semi fowler’s position.
- If the patient cannot expectorate, give suction to clear the airway.
- Administer oxygen if needed and as ordered by a physician.
- Give the TB patients fluids to loosen up secretions for easier expulsion from the lungs.
- Instruct patient to give up smoking.
- Provide balanced and vitamin containing diets as prescribed.
- Maintain fluid intake at least 2500ml per day unless indicated.
- Ensure plenty of rest.
- Administer all medication as ordered at the exact time on an empty stomach.
- Explain to a patient about doses of medicine, frequency of administration, expected action and outcome, and the reasons for the long treatment period.
- Explain to the patient about the side effect of TB drug (High color urine).
- Carefully monitor any complications or adverse effects of the drug.
- Refer patients having a hard time sticking to their drug therapy for direct observation therapy, where someone will watch them take their medication as they should.
- Encourage the patient to stay out of the workplace, school, and public place until the physician declared that it is now safe and not spread to others.
- Teach patients how to avoid spreading the disease by sneezing or coughing into doubly ply tissue instead of their bare hands, washing their hands after this, and disposing of the tissue into a closed plastic bag.
- Teach the tuberculosis patient to stay in well-ventilated areas and limit contact with other people to avoid spreading the infection.
- Encourage clients to accommodate their sputum when coughing to prevent transmission of infection.
- Monitor the patient’s weight daily.
More questions related to this topic:
- Pulmonary Tuberculosis: Types, Symptoms & Treatments.
- Tuberculosis (Pulmonary Tuberculosis)-Symptoms.
- Tuberculosis Causes, Symptoms, Treatment.
- Pulmonary Tuberculosis – Treatment – Step-by-Step.
- CDC | TB | Basic TB Facts | Signs & Symptoms of TB Disease.
- What is the Cause of Pulmonary Tuberculosis?
- Is Tuberculosis Contagious?
- Can You Die of Tuberculosis?
- Is Tuberculosis Curable Disease?
- Tuberculosis Symptoms, Causes & Risk Factors.
- Pulmonary Tuberculosis Diet.
- Pulmonary Tuberculosis Definition.
- Classification of Pulmonary Tuberculosis Disease (TB).
- Tuberculosis (TB) – Symptoms.
- Pulmonary Tuberculosis Diagnosis.
- Pulmonary Tuberculosis Treatment.
- Pulmonary Tuberculosis Precautions.

Maria Khatun Mona is a Founder and Editor of Nursing Exercise Blog. She is a Nursing and Midwifery Expert. Currently she is working as a Registered Nurse at Evercare Hospital, Dhaka, Bangladesh. She has great passion in writing different articles on Nursing and Midwifery. Mail her at “maria.mona023@gmail.com”
