Definition of Diabetes Mellitus Disease:
Diabetes mellitus disease is commonly referred to as a group of metabolic diseases characterized by hyperglycemia resulting from insufficiency secretion of insulin, less insulin action, or both.
Types of Diabetes Mellitus Disease or Classification of Diabetes Mellitus:
There are three major types of diabetes which are discussed below:
1. Type-1 Diabetes Mellitus Disease or Diabetes Mellitus Type 1:
Type- 1 Diabetes Mellitus is known as Insulin Dependent Diabetes Mellitus (IDDM) or Juvenile diabetes. Pancreases fail to produce enough beta cells or insulin.
2. Type-2 Diabetes Mellitus Disease or Diabetes Mellitus Type 2:
Type-2 Diabetes Mellitus is known as Non-Insulin Dependent Diabetes (NIDDM), beta cells produce insufficient Insulin.
3. Gestational Diabetes Disease:
Insufficient production of insulin during pregnancy by the mother. This diabetes recovers following pregnancy, but they are at risk for developing type -2 diabetes mellitus later in life.
Sign and Symptoms of Diabetes Mellitus Disease or Diabetes Mellitus Symptoms:
Sign and symptoms of diabetes mellitus are the following:
For Type-1 Diabetes Mellitus Disease:
- Fast onset because of no insulin-producing,
- Polyphagia ( increased appetite),
- Polydipsia ( increased thirst),
- Polyurea ( increased urination ),
- Unexplained Weight loss,
- Frequent genital infections ( Balanitis/ vaginitis),
- Delay healing process,
- Dry mouth.
For Type-2 Diabetes Mellitus Disease:
- Slow onset because of some insulin-producing,
- Polyurea,
- Polydipsia,
- Candidal infection,
- Delay healing process,
- Blurred vision,
- Lower extremities parenthesis,
- Headache,
- Extremely fatigue,
- Dehydration.
Causes of Diabetes Mellitus Disease:
There are different causes for diabetes mellitus which are in the below:
For Type-1 Diabetes Mellitus Disease:
- Type-1 diabetes mellitus is caused by the destruction of the beta cells of the pancreas and when the beta cells are destroyed, the pancreas unable to produce insulin at all.
- Viral infection of the pancreas.
- Autoimmune disease.
For Type-2 Diabetes Mellitus Disease:
- Type-2 diabetes mellitus is caused by insufficient production of insulin by the pancreas, sometimes the amount of insulin is normal but the tissue is resistant to glucose,
- Heredity,
- Obesity,
- Long time use of steroid, phenytoin, thiazide diuretics,
- Thyroid hormone dysfunction,
- Severe or recurrent pancreatitis,
- Acromegaly,
- Lack of physical activity,
- Cancer of the pancreas.
Diagnosis for Diabetes Mellitus Disease:
Various diagnosis ways for diabetes mellitus are mentioned below:
For Type-1 Diabetes Mellitus Disease:
- Fasting blood/ plasma glucose level (FBS) more than 126mg/dl ( 7.0mmol/L)
- 2 hours of breakfast plasma glucose level of more than 200mg/dl ( 11.1mmol/L)
- OGTT( Oral glucose tolerance test)
- Random plasma/ blood glucose ( RBS)
For Type-2 Diabetes Mellitus Disease:
- Fasting blood/ plasma glucose level (FBS) more than 126mg/dl ( 7.0mmol/L),
- 2 hours of breakfast plasma glucose level more than 200mg/dl ( 11.1mmol/L),
- Random plasma/ blood glucose ( RBS),
- Hba1c,
- TSH ( thyroid-stimulating hormone test),
- FT3 and FT4.
Treatment for Diabetes Mellitus:
There are different treatment processes for diabetes mellitus. Those are in the following:
For Type-1 Diabetes Mellitus Disease:
Treatment of type-1 involves diet and exercise.
- Dietary Management and Physical Exercise:
Dietary management and exercise are typically the first steps toward reducing blood sugar levels. Dietary carbohydrate and activity must be co-ordinated with insulin action so that-
- Insulin is available for optimal metabolism when the food that was eaten is absorbed.
- Food is available while insulin is acting to prevent hypoglycaemic reactions.
- Insulin therapy:
- Rapid-acting (Aspart, Lispro, Glucolize),
- Short-acting (Regular).
- Intsermediate acting (Neutral protamine hegadorn)
- Long acting (Luntus, Levemir).
- Continuous subcutaneous insulin ( CSII) –Rapid-acting insulin infused continuously 24 hours through an insulin pump, at 1 or more basal rates.
For Type-2 Diabetes Mellitus Disease:
Type-2 DM is treated first with weight reduction, a diabetic diet, and exercise. When these first measures fail to control hyperglycemia, oral medications are to be used.
The oral medications are-
- Sulfonylureas:
which stimulates the release of insulin from pancreatic islets, reduces blood glucose. Those are chlorpropamide, glyburide, glipizide.
- Meglitinides:
Stimulate a rapid or short-lived release of insulin from the pancreas such as repaglinide, metformin.
- Alpha-glucosidase
- Glinides.
- Insulin secretagogues.
- Incretines.
- Thiazolidione
- Boguanide
Prevention for Diabetes Mellitus Disease:
There are different ways of preventing diabetes mellitus which are mentioned below:
- Maintain a better healthy lifestyle.
- Eat a healthy diet.
- Control of body weight.
- Turn off the television and computer and get more physical activity.
- Take whole grains and whole grains products over highly processed carbohydrates.
- Avoid sugary drinks and choose water, coffee, or tea instead.
- Eat good fats instead of bad fats.
- Limit red meat and choose nuts, whole grains, poultry, or fish.
- No smoking.
- Regular monitor of blood glucose.
- Taking care of body especially eye and food.
- Check feet to make sure there is no nerve damage or interruption of blood flow.
- Consult with a physician at least once a month when the age for more than 45 years.
- Monitor and control blood pressure.
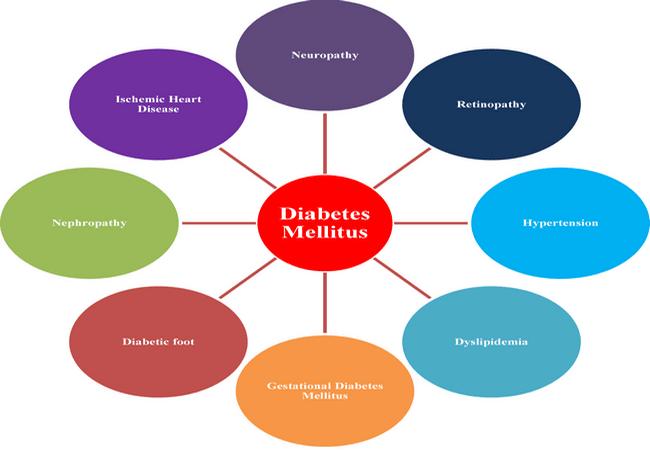
Complications of Diabetes Mellitus Disease:
Various complications of diabetes mellitus are in the below:
- Hyperglycaemia,
- Hypoglycemia,
- Diabetic ketoacidosis,
- Hyper-osmolar hyperglycaemic non-kenotic syndrome (HONK syndrome),
- Cardiovascular disease,
- Cerebro-vascular disease,
- Diabetic neuropathy,
- Diabetic nephropathy male erectile dysfunction.
Nursing Intervention for Diabetes Mellitus Disease:
There are different types of nursing intervention for diabetes mellitus which are mentioned in the following:
- Monitor and control blood sugar.
- Monitor body weight daily.
- Provide a diabetic diet and determine the diet and eating patterns and compare with blood glucose.
- Collaboration with dieticians about patient diet.
- Administer medications and insulin properly.
- Collaboration examination of blood sugar with insulin therapy.
- Observe the signs of hypoglycemia such as changes in the level of consciousness; skin moist/cold, rapid pulse, hunger, sensitivity to stimuli, anxiety, and headache.
- Teach patient and family about hypoglycemia and hypoglycaemic sign symptoms.
- Observe for the signs of infection and inflammation: fever, flushed appearance, wound drainage, purulent sputum, and cloudy urine.
- Promote and teach good hand hygiene.
- Provide feet care (observe and investigate reports of hyperesthesia, pain, or sensory loss in the feet or legs) and teach how to care for feet.
- Recommended regular ophthalmologic examination.
- Investigate and check for ulcers, reddened areas, pressure points, loss of pedal pulses.
- Provide skincare: keep skin dry, gently massage bony areas.
- Keep bed sheets dry, tidy, and wrinkle-free.
- Careful wound care.
- Maintain asepsis technique during IV insertion, administering of medications, check any swelling and redness, and change IV sites as indicated.
- Provide cognitive and emotional support to the patient.
- Teach about home care and control of blood sugar.
- Monitor laboratory values: blood glucose, serum osmolality, Hb/Hct, BUN/Cr.
- Carry out the prescribed regimen for correcting DKA as indicated.
- Assist the patient to develop coping strategies and discuss with the patient the need for activity and help inactivity in daily living.
- Encourage the patient to do some exercises to control blood sugar.
- Treat hypoglycaemic reactions promptly by giving sugar, juice, hard candy, honey, or IV dextrose.
- Keep accurate records of vital signs, fluid intake, urine output, and caloric intake.
- Check sign symptoms of complication diabetic effects.
- Observe for signs of the urinary tract and vaginal infections, and monitor urinary protein and early signs of nephropathy.
More questions related to this topic:
- Diabetes Mellitus: Types, Symptoms, Causes, Treatments.
- Diabetes Mellitus: An Overview.
- Diabetes Mellitus Definition.
- What Type of Disease is Diabetes?
- What are the Two Major Types of Diabetes Mellitus?
- What are the Symptoms of a Diabetic Person?
- Why Do People Get Diabetes?
- What is Type 1 Diabetes Mellitus?
- What is Type 2 Diabetes Mellitus?

Maria Khatun Mona is a Founder and Editor of Nursing Exercise Blog. She is a Nursing and Midwifery Expert. Currently she is working as a “Senior Staff Nurse” at “Dinajpur Medical College Hospital”, Bangladesh. She has great passion in writing different articles on Nursing and Midwifery. Mail her at “maria.mona023@gmail.com”

My wife diabetes symptom was diabetic neuropathy. We didn’t know she was diabetic until we went to my doctor complaining about constant foot pain. After a multitude of tests for everything from rheumatoid arthritis to muscular dystrophy, an emergency room physician checked her blood sugar.After reviewing a letter written by my doctor, where I read he had prescribed Celebrex for her due to pain of Arthritis which had really messed her neck, back and knees, I found that one of the side effects of Celebrex is Diabetes, my wife was able to effectively cure herbal condition multivitamincare org It is too much for a patient to endure such as they slowly begin to pass away if the right medication is not taken organic herbal treatment.Having a positive mind is a powerful tool .My prayers goes out to diabetes patients and their care givers.